Prevalence and Outcome of Preterm Neonates Admitted to Neonatal Unit of a Tertiary Care Center in Western Nepal
DOI:
https://doi.org/10.22502/jlmc.v6i2.218Keywords:
Gestational Age, NICU, Preterm Neonates, Neonatal UnitAbstract
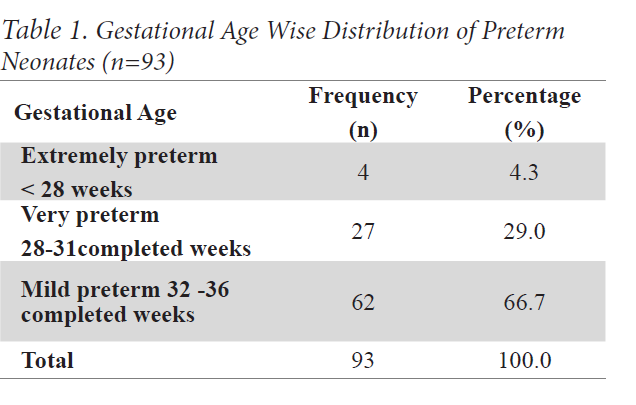
Introduction: Preterm deliveries contribute to major morbidity and mortality in developing countries. They are a leading cause of admission in neonatal care units. Advances in the management have ensured better survival of preterm births, however cost, care and resource limitations influence the outcome.This study was conducted to determine the prevalence, risk factors, morbidity patterns and outcome of preterm admissions to a neonatal unit of a tertiary care center. Methods: This was a retrospective study where all preterm admissions over a period of two years were evaluated for maternal risk factors and morbidity pattern. Outcome was measured in terms of survival rate and case fatality rate. Mann Whitney U test and Fisher's Exact test were used to see the association between various parameters and clinical outcome. Results: Preterm admissions constituted16.48% of all neonatal unit admissions with a male to female ratio of 1.32:1. Common risk factors for preterm births were Prelabour Rupture of Membrane (31.2%) followed by Hypertensive Disorders in Pregnancy (15.1%) and Antepartum Hemorrhage (8.6%). Common morbidities were Sepsis (40.9%), Jaundice (28%) and Respiratory Distress Syndrome (RDS) (14%). Case fatality rate was significantly high in RDS (45.1%) and perinatal asphyxia (11.1%). Overall survival rate was 75.26%. Conclusion: Preterm births were an important cause for admissions in neonatal unit. Sepsis, jaundice, RDS and necrotizing enterocolitis were common morbidities observed. Since clinical outcome was related to gestational age, improving antenatal care, timely interventions and early referral of high risk pregnancies to tertiary level centers might improve the survival rate
Downloads
References
Howson ECP, Kinney MV, Lawn JE. March of Dimes, PMNCH, Save the Children, WHO. Born Too Soon: The Global Action Report on Preterm Birth. [Internet] World Health Organization. Geneva, 2012. Available From: http://www.who.int/pmnch/media/news/2012/201204_borntoosoon-report.pdf
US Agency for International Development. Nepal: Profile of preterm and low birth weight prevention and care [Internet]. USAID; 2015. Available from: https://reliefweb.int/sites/reliefweb.int/files/resources/Nepal_2.pdf
Butler AS, Behrman RE, editors. Preterm birth: causes, consequences, and prevention. National Academies Press; 2007 May 23. Available from: https://www.ncbi.nlm.nih.gov/books/NBK11362/pdf/Bookshelf_NBK11362.pdf
Barton L, Hodgman JE, Pavlova Z. Causes of death in the extremely low birth weight infant. Pediatrics. 1999 Feb 1;103(2):446-51. PMID: 9925839 DOI: 10.1542/peds.103.2.446 [Publisher Full Text]
Lindström K. Long-term consequences of preterm birth: Swedish National Cohort Studies. Inst för klinisk forskning och utbildning, Södersjukhuset/Dept of Clinical Science and Education, Södersjukhuset; 2011 May 6. [Publisher Full Text]
Lumley J. Defining the problem: the epidemiology of preterm birth. BJOG: An International Journal of Obstetrics & Gynaecology. 2003 Apr;110 Suppl 20:3-7. PMID: 12763104 DOI: 10.1046/j.1471-0528.2003.00011.x [Publisher Full Text]
Ballard JL, Novak KK, Driver M. A simplified score for assessment of fetal maturation of newly born infants. The Journal of pediatrics. 1979 Nov 1;95(5):769-74. PMID: 490248
Kliegman, R., Stanton, B., St. Geme, J., Schor, N., Behrman, R. and Nelson, W. (2016). Nelson textbook of pediatrics. Philadelphia: Elsevier; 2016. P. 517
Kliegman, R., Stanton, B., St. Geme, J., Schor, N., Behrman, R. and Nelson, W. (2016). Nelson textbook of pediatrics. Philadelphia: Elsevier; 2016. P 636-7.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, Brotherton T. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Annals of surgery. 1978 Jan;187(1):1-7. PMID: 490248 [Publisher Full Text]
Gupta A, Shetty D, Madhava KK. Prevalence and Consequences of Preterm Admissions at the Neonatal Intensive Care Unit of tertiary care centre in South India: a retrospective study. International Journal of Current Advanced Research. 2017 May 28; 06(05):3728-30. DOI: 10.24327/ijcar.2017.3730.0357 [Publisher Full Text]
Kunle-Olowu OE, Peterside O, Adeyemi OO. Prevalence and outcome of preterm admissions at the neonatal unit of a tertiary health centre in Southern Nigeria. Open Journal of Pediatrics. 2014 Mar 6;4(01):67. DOI: 10.4236/ojped.2014.41009 [Publisher Full Text]
Ugwu GI. Pattern of morbidity and mortality in the newborn special care unit in a tertiary institution in the Niger Delta region of Nigeria: A two year prospective study. Global Advanced Research Journal of Medicine and Medical Sciences. 2012 Jul;1(6):133-8.
Kuppusamy N, Vidhyadevi A. Prevalence of Preterm Admissions and the Risk Factors of Preterm Labor in Rural Medical College Hospital. Int J Sci Stud. 2016 Dec 1;4(9):125-8. DOI: 10.17354/ijss/2016/629 [Publisher Full Text]
Chowdareddy N, Kumar YC, Thomas A, Deepthi KU, Ravichander M. Mortality pattern of preterm infants and etiological factors of preterm births in rural tertiary care centre: A retrospective study. International Journal of Scientific and Research Publications. 2014 Mar;4(3):2-3. [Publisher Full Text]
Orbach H, Matok I, Gorodischer R, Sheiner E, Daniel S, Wiznitzer A, Koren G, Levy A. Hypertension and antihypertensive drugs in pregnancy and perinatal outcomes. American journal of obstetrics and gynecology. 2013 Apr 1;208(4):301-e1-6. PMID: 23159698 DOI: 10.1016/j.ajog.2012.11.011
Shrestha S, Dangol SS, Shrestha M, Shrestha RP. Outcome of preterm babies and associated risk factors in a hospital. Journal of the Nepal Medical Association. 2010 Oct 1;50(180):286-90. PMID: 22049892
Uma S, Nisha S, Shikha S. A prospective analysis of etiology and outcome of preterm labor. Journal of Obstetrics and Gynecology of India. 2007 Jan 1;57(1):48-52.
Onalo R, Olateju KE. Trend and Seasonality in Admissions and Outcome of Low Birth Weight Infants in Gwagalada Abuja, Nigeria. International Journal of Tropical Disease and Health. 2013;3(3):190-8. [Publisher Full Text]
Khan MR, Maheshwari PK, Shamim H, Ahmed S, Ali SR. Morbidity pattern of sick hospitalized preterm infants in Karachi, Pakistan. Journal of the Pakistan Medical Association. 2012;62(4):386-88. PMID: 22755286 [Publisher Full Text]
Downloads
Published
Issue
Section
License
- The Journal of Lumbini Medical College (JLMC) publishes open access articles under the terms of the Creative Commons Attribution (CC BY) License which permits use, distribution and reproduction in any medium, provided the original work is properly cited.
- JLMC requires an exclusive licence to publish the article first in its journal in print and online.
- The corresponding author should read and agree to the following statement before submission of the manuscript for publication,
- License agreement
- In submitting an article to Journal of Lumbini Medical College (JLMC) I certify that:
- I am authorized by my co-authors to enter into these arrangements.
- I warrant, on behalf of myself and my co-authors, that:
- the article is original, has not been formally published in any other peer-reviewed journal, is not under consideration by any other journal and does not infringe any existing copyright or any other third party rights;
- I am/we are the sole author(s) of the article and have full authority to enter into this agreement and in granting rights to JLMC are not in breach of any other obligation;
- the article contains nothing that is unlawful, libellous, or which would, if published, constitute a breach of contract or of confidence or of commitment given to secrecy;
- I/we have taken due care to ensure the integrity of the article. To my/our - and currently accepted scientific - knowledge all statements contained in it purporting to be facts are true and any formula or instruction contained in the article will not, if followed accurately, cause any injury, illness or damage to the user.
- I, and all co-authors, agree that the article, if editorially accepted for publication, shall be licensed under the Creative Commons Attribution License 4.0. If the law requires that the article be published in the public domain, I/we will notify JLMC at the time of submission, and in such cases the article shall be released under the Creative Commons 1.0 Public Domain Dedication waiver. For the avoidance of doubt it is stated that sections 1 and 2 of this license agreement shall apply and prevail regardless of whether the article is published under Creative Commons Attribution License 4.0 or the Creative Commons 1.0 Public Domain Dedication waiver.
- I, and all co-authors, agree that, if the article is editorially accepted for publication in JLMC, data included in the article shall be made available under the Creative Commons 1.0 Public Domain Dedication waiver, unless otherwise stated. For the avoidance of doubt it is stated that sections 1, 2, and 3 of this license agreement shall apply and prevail.
Please visit Creative Commons web page for details of the terms.