Perceived Barriers to Adherence to Standard Precautions among Healthcare Personnel Working in a Teaching Hospital of Palpa District, Nepal
DOI:
https://doi.org/10.22502/jlmc.v7i2.295Keywords:
Adherence, Barrier, Healthcare personnel, Standard precautionAbstract
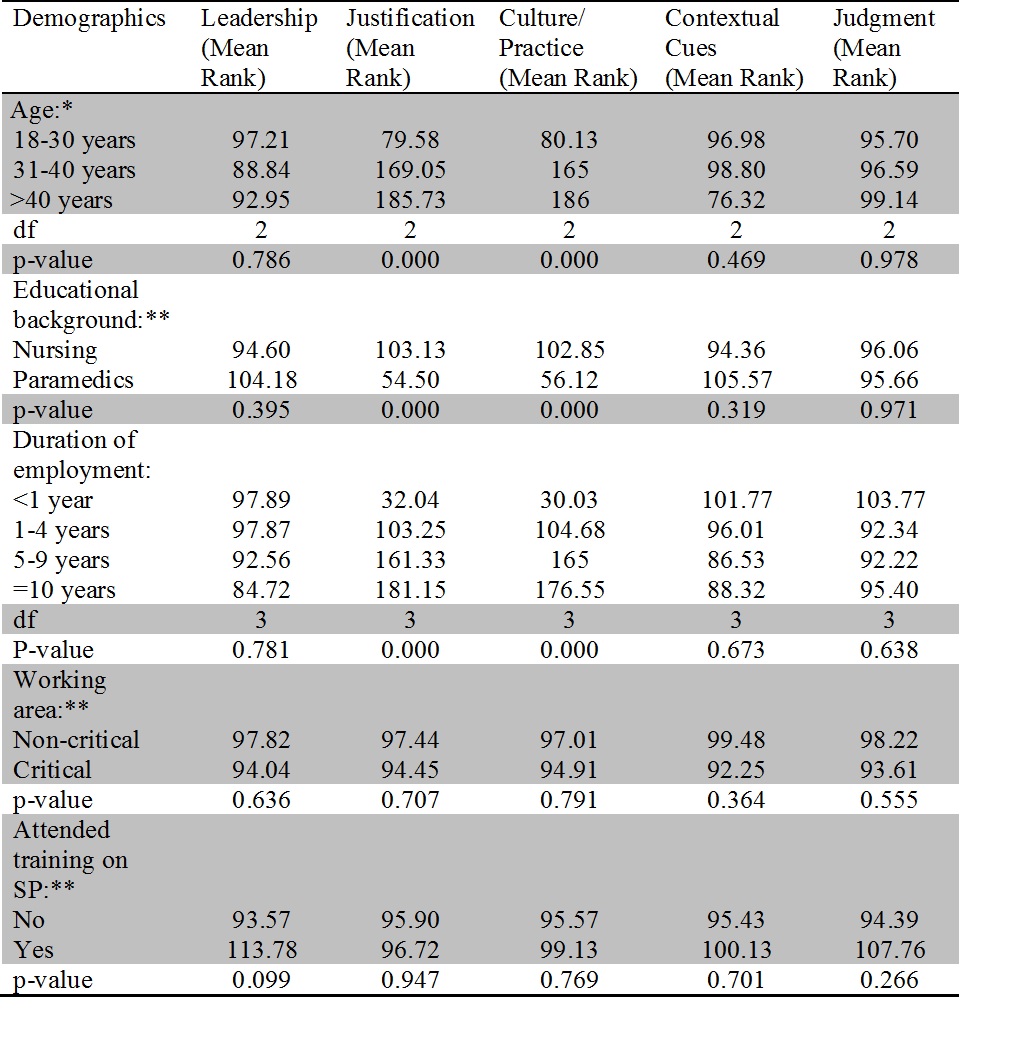
Introduction: The present study aimed to find out the perceived barriers to adherence to standard precautions among healthcare personnel working in a teaching hospital of Palpa district. Methods: A descriptive cross-sectional study was conducted among 191 healthcare personnel in April 2019. Barriers to standard precautions adherence were evaluated using ‘Factors Influencing Adherence to Standard Precautions Scale’. Mann Whitney U test and Kruskal Wallis H test were applied to examine the association of selected demographic variables: age, educational background, duration of employment, working areas and having attended trainings related to standard precautions with the perceived barriers to standard precautions adherence. Results: The mean age of participants was 24.87±6.05 years. Most (85.3%) of participants were nurses. 19.9% and 52.4% of participants always performed hand hygiene before and after using personal protective equipment respectively. The subscale scores in leadership and culture of the institute were 14.86±4.21 (possible range 0-24) and 14.59±2.60 (possible range 0-20) respectively. Subscale scores in judgement and contextual cues were 17.49±3.46 (possible range 0-20) and 18.02±5 (possible range 0-24) respectively. Score in justification was 7.52±5.12 (possible range 0-28). Age, educational background and duration of employment had a statistically significant association with subscale scores on justification and perceived culture of the institution. Conclusion: The present study revealed that only 19.9% of the participants would perform hand hygiene before using gloves and 52.4% of participants would do it afterwards. Personal judgement, dependence on contextual cues and inadequate leadership skills were found to be the major barriers to adherence to standard precautions.
Downloads
References
Mutters NT, Tacconelli E. Infection prevention and control in Europe - the picture in the mosaic. Clin Microbiol Infect. 2015;21(12):1045–6. PMID: 26100372. DOI:https://doi.org/10.1016/j.cmi.2015.06.012
Lopchan M, Gurung G, Rajbanshi L, Osti C, Baniya A. Knowledge and Attitude Towards Infection Control Among Supporting Staffs of Chitwan Medical College, Bharatpur, Chitwan. Journal of Chitwan Medical College. 2016;6(15):40–7. Available from: http://www.cmc.edu.np/images/gallery/ Original%20Articles/Sx6E99.pdf
World Health Organization. Report on the Burden of Endemic Health Care-Associated Infection Worldwide. World Health Organization. ISBN: 9789241501507, 2011. Available from: https://apps.who.int/iris/ handle/10665/80135
Joshi SC, Diwan V, Tamhankar AJ, Joshi R, Shah H, Sharma M, et al. Staff perception on biomedical or health care waste management: a qualitative study in a rural tertiary care hospital in India. PLoS One. 2015;10(5):1- 15. PMID: 26023783. DOI:https://doi.org/10.1371/journal.pone.0128383
Joshi SC, Diwan V, Joshi R, Sharma M, Pathak A, Shah H, et al. “How Can the Patients Remain Safe, If We Are Not Safe and Protected from the Infections� A Qualitative Exploration among Health-Care Workers about Challenges of Maintaining Hospital Cleanliness in a Resource Limited Tertiary Setting in Rural India. Int J Environ Res Public Health. 2018;15(9):1-14. PMID: 30200603. DOI: https://doi.org/10.3390/ijerph15091942
World Health Organization. Fact sheet World Health Organization. Available from: http://www.who.int/gpsc/country_work/ gpsc_ccisc_fact_sheet_en.pdf [Accessed on 23rd July 2019].
Bouchoucha SL, Moore KA. Factors Influencing Adherence to Standard Precautions Scale: A psychometric validation. Nurs Heal Sci. 2019;21(2):178- 85. PMID: 30362238. DOI:https://doi.org/10.1111/nhs.12578
Basnyat B, Pokharel PK, Dixit SM, Karkey A, Shrestha B, Khanal B, et al. Situation Analysis and Recommendations: Antibiotic use and Resistance in Nepal. Nepal Public Health Foundation. 2015 Available from: https://cddep.org/wp-content/uploads/2017/06/ garp_nepal_sitan_execsum-1.pdf
Shrestha A, Bhattarai D, Thapa B, Basel P, Wagle RR. Health care workers’ knowledge, attitudes and practices on tuberculosis infection control, Nepal. BMC Infect Dis. 2017;17(1):1-7. PMID: 29149873. DOI:https://doi.org/10.1186/s12879-017-2828-4
Amatya R, Shrestha B, Shrestha T. Infection Prevention and Health Care Waste Management Training Course. National Health Training Centre. 2017;2-2
Bennett L, Dahal DR, Govindasamy P. Caste, Ethnic and Regional Identity in Nepal: Further Analysis of the 2006 Nepal Demographic and Health Survey.USA: Macro International Inc. 2008. Available from: https://dhsprogram.com/pubs/pdf/ FA58/FA58.pdf
Zhou Y, Zhang D, Chen Y, Zhou S, Pan S, Huang Y, et al. Healthcare-associated infections and Shanghai clinicians: A multicenter cross-sectional study. PLoS One. 2014;9(8):e105838. PMID: 25148526. DOI:http://doi.org/10.1371/journal.pone.0105838
Hessels AJ, Larson EL. Relationship between patient safety climate and standard precaution adherence: a systematic review of the literature. The Journal Hospital Infection. 2016;92(4):349-62. DOI: http://dx.doi.org/10.1016/j.jhin.2015.08.023
Pranita D, Mediawati AS, Mirwanti R. Perceived Barriers toward Standard Precautions Implementations among Nurses in the Emergency Department. Journal of Nursing Care. 2019;2(3):178-92. Available from: https://bit.ly/37sJi3X
Ohara H, Pokhrel BM, Dahal RK, Mishra SK, Kattel HP, Shrestha DL, et al. Fact-finding Survey of Nosocomial Infection Control in Hospitals in Kathmandu, Nepal — A Basis for Improvement. Trop Med Health. 2013;41(3):113–9. PMID: 24155652. DOI:https://doi.org/10.2149/tmh.2013-03
Kim E, Jeong I, Thanju S. Knowledge, Attitude, and Compliance of Healthcare-associated Infection Control among Nurses in the Western Development Region, Nepal. Korean Journal of Nosocomial Infection Control. 2016;21(1):9–17. DOI: https://doi.org/10.14192/kjnic.2016.21.1.9
Siegel JD, Rhinehart E, Jackson M, Chiarello L; Health Care Infection Control Practices Advisory Committee. 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings. Am J Infect Control. 2007;35(10 Suppl 2): S65-164. PMID: 18068815. DOI:https://doi.org/10.1016/j.ajic.2007.10.007
Mitchell KF, Barker AK, Abad CL, Safdar N. Infection control at an urban hospital in Manila, Philippines: a systems engineering assessment of barriers and facilitators. Antimicrob Resist Infect Control. 2017;6:1- 9. PMID: 28883912. DOI:http://doi.org/10.1186/s13756-017-0248-2
Landefeld J, Sivaraman R, Arora NK. Barriers to Improving Patient Safety in India: Focus Groups with Providers in the Southern State of Kerala. Indian J Community Med. 2015;40(2):116–20. PMID: 25861173. DOI: https://doi.org/10.4103/0970-0218.153875
Barker AK, Brown K, Siraj D, Ahsan M, Sengupta S, Safdar N. Barriers and facilitators to infection control at a hospital in northern India: A qualitative study. Antimicrob Resist Infect Control. 2017;6:1–7. PMID: 28405312. DOI: https://doi.org/10.1186/s13756-017-0189-9
Birgand G, Johansson A, Szilagyi E, Lucet JC. Overcoming the obstacles of implementing infection prevention and control guidelines. Clin Microbiol Infect. 2015;21(12):1067– 71. PMID: 26369604. DOI: https://doi.org/10.1016/j.cmi.2015.09.005
Stalpers D, De Vos MLG, Van Der Linden D, Kaljouw MJ, Schuurmans MJ. Barriers and carriers: a multicenter survey of nurses ’ barriers and facilitators to monitoring of nurse-sensitive outcomes in intensive care units. Nurs Open. 2017;4(3):149–56. PMID: 28694979. DOI:https://doi.org/10.1002/nop2.85
Oh E, Choi JS. Factors influencing the adherence of nurses to standard precautions in South Korea hospital settings. Am J Infect Control. 2019;47(11):1346–51. PMID: 31324494. DOI:https://doi.org/10.1016/j.ajic.2019.05.015
Akagbo SE, Nortey P, Ackumey MM. Knowledge of standard precautions and barriers to compliance among healthcare workers in the Lower Manya Krobo District, Ghana. BMC Res Notes. 2017;10(1):1– 9. PMID: 28854982. DOI: https://doi.org/10.1186/s13104-017-2748-9
Downloads
Published
Issue
Section
License
- The Journal of Lumbini Medical College (JLMC) publishes open access articles under the terms of the Creative Commons Attribution (CC BY) License which permits use, distribution and reproduction in any medium, provided the original work is properly cited.
- JLMC requires an exclusive licence to publish the article first in its journal in print and online.
- The corresponding author should read and agree to the following statement before submission of the manuscript for publication,
- License agreement
- In submitting an article to Journal of Lumbini Medical College (JLMC) I certify that:
- I am authorized by my co-authors to enter into these arrangements.
- I warrant, on behalf of myself and my co-authors, that:
- the article is original, has not been formally published in any other peer-reviewed journal, is not under consideration by any other journal and does not infringe any existing copyright or any other third party rights;
- I am/we are the sole author(s) of the article and have full authority to enter into this agreement and in granting rights to JLMC are not in breach of any other obligation;
- the article contains nothing that is unlawful, libellous, or which would, if published, constitute a breach of contract or of confidence or of commitment given to secrecy;
- I/we have taken due care to ensure the integrity of the article. To my/our - and currently accepted scientific - knowledge all statements contained in it purporting to be facts are true and any formula or instruction contained in the article will not, if followed accurately, cause any injury, illness or damage to the user.
- I, and all co-authors, agree that the article, if editorially accepted for publication, shall be licensed under the Creative Commons Attribution License 4.0. If the law requires that the article be published in the public domain, I/we will notify JLMC at the time of submission, and in such cases the article shall be released under the Creative Commons 1.0 Public Domain Dedication waiver. For the avoidance of doubt it is stated that sections 1 and 2 of this license agreement shall apply and prevail regardless of whether the article is published under Creative Commons Attribution License 4.0 or the Creative Commons 1.0 Public Domain Dedication waiver.
- I, and all co-authors, agree that, if the article is editorially accepted for publication in JLMC, data included in the article shall be made available under the Creative Commons 1.0 Public Domain Dedication waiver, unless otherwise stated. For the avoidance of doubt it is stated that sections 1, 2, and 3 of this license agreement shall apply and prevail.
Please visit Creative Commons web page for details of the terms.