Clinical Profile and Short-term Outcome of Heart Failure Patients in a Tertiary Hospital in Kaski, Nepal: A Cross-sectional Study
DOI:
https://doi.org/10.22502/jlmc.v10i1.495Keywords:
Clinical profile, Heart failure, HospitalizationAbstract
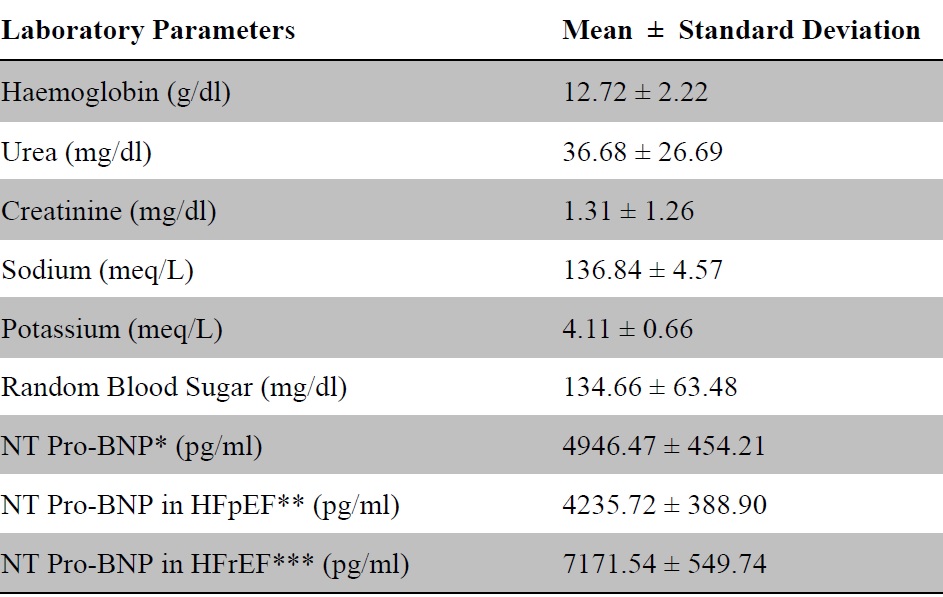
Introduction: Heart failure is one of the leading causes of hospitalization. The aim of this study was to evaluate the epidemio-clinical profile and short-term outcome of hospitalized heart failure patients in a tertiary care hospital. Methods: This descriptive cross-sectional study was conducted at Pokhara Academy of Health Sciences, Kaski, Nepal from October 1, 2021 to January 31, 2022. All the hospitalized heart failure patients aged 18 years or above were included. Relevant history, examination, laboratory, and pertinent findings were noted. Descriptive statistics were used for qualitative and quantitative data. Paired t-test was used for the comparison of pre-and post-hospitalization data. A p-value <0.05 was taken for statistical significance. Results: There were a total of 116 patients (65.5% females) with a mean age of 64.20 ± 16.35 years. Most of them had shortness of breath (97.4%) and orthopnea (72.4%) and presented with pedal/sacral edema (81.9%) and bilateral basal crepitations (69.8%) in the chest. Heart failure with preserved ejection fraction was the most prevalent (61.2%) type and dilated cardiomyopathy (27.6%) was the commonest etiology of heart failure. The median duration of hospitalization was five days and the in-hospital mortality was 2.6%. Loop diuretics and vasodilators (angiotensin-converting enzyme inhibitor/angiotensin receptor blocker) were the most commonly used medications. Conclusions: Dilated cardiomyopathy was the most common etiology and heart failure with preserved ejection fraction was the predominant type of heart failure. With a short length of stay and low in-hospital mortality, the short-term outcome was good.
Downloads
References
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur eart J. 2016;37(27):2129-2200 PMID: 27206819. DOI: https://doi.org/10.1093/eurheartj/ehw128
Ferreira JP, Metra M, Mordi I, Gregson J, Maaten JMT, Tromp J, et al. Heart failure in the outpatient versus inpatient setting: findings from the BIOSTAT-CHF study. Eur J Heart Fail. 2019;21(1):112-20 PMID: 30338883 DOI: https://doi.org/10.1002/ejhf.1323
Fonarow GC, Abraham WT, Albert NM, Gattis WA, Gheorghiade M, Greenberg BH, et al. Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF): rationale and design. Am Heart J. 2004;148(1):43-51 PMID: 15215791. DOI: https://doi.org/10.1016/j.ahj.2004.03.004
Bhattarai M, Shah RK, Sainju NK, Bhandari B, Keshari S, Karki DB. Etiological spectrum of heart failure in a tertiary health care facility of Central Nepal. Nepalese Heart Journal. 2019;16(2):23-8 DOI: https://doi.org/10.3126/njh.v16i2.26313
Gheorghiade M, Abraham WT, Albert NM, Greenberg BH, O’Connor CM, She L, et al. Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure. JAMA. 2006;296(18):2217-26 PMID: 17090768 DOI: https://doi.org/10.1001/jama.296.18.2217
Regmi SR, Maskey A, Dubey L. Heart Failure Study: Profile of Heart Failure Admissions in Medical Intensive Care Unit. Nepalese Heart Journal. 2017;6(1):32-4 DOI: https://doi.org/10.3126/njh.v6i1.18452
Dubey L, Sharma SK, Chaurasia AK. Clinical profile of patients hospitalized with heart failure in Bharatpur, Nepal. J Cardiovasc Thorac Res. 2012;4(4):103-5 PMID: 24250996 DOI: https://doi.org/10.5681/jcvtr.2012.025
Sharma D, Kafle RC, Alurkar VM. Pattern of cardiovascular disease among admitted in tertiary care teaching hospital. J Nepal Health Res Counc. 2020;18(46):93-8 PMID: 32335600 DOI: https://doi.org/10.33314/jnhrc.v18i1.2156
Shrestha UK, Alurkar VM, Baniya R, Barakoti B, Poudel D, Ghimire S. Profiles of heart failure in the western region of Nepal: prognostic implications of the MELD-XI score. Internal Medicine Inside. 2015;3(0):1 DOI: http://dx.doi.org/10.7243/2052-6954-3-1
Adhikari S, Gajurel RM, Poudel CM, Shrestha H, Thapa S, Devkota S, et al. Precipitating factors leading to decompensation of heart failure in patients attending a tertiary care centre of Nepal. Nepalese Heart Journal. 2020;17(1):17-21 DOI: https://doi.org/10.3126/njh.v17i1.28798
Shareef M, KC MB, Raut R, Hirachan A, KC B, Agarwal AK, et al. Etiology of heart failure in the emergency department of a tertiary cardiac centre of Nepal. Nepalese Heart Journal. 2017;14(2):1-4 DOI: https://doi.org/10.3126/njh.v14i2.18494
Dhungana SP, Chaparia A, Sharma SK. Prevalence of co-morbid conditions in Heart failure: an experience at tertiary care hospital. Journal of Nobel Medical College. 2018;6(2):35-41 DOI: https://doi.org/10.3126/jonmc.v6i2.19568
Monib AK, Dhungana SP, Nepal R, Ghimire R. Clinical Profile of Patients with Heart Failure in Eastern Part of Nepal: a Hospital based study. Journal of Nobel Medical College. 2019;8(1):48-52 DOI: https://doi.org/10.3126/jonmc.v8i1.24477
Kligfield P, Gettes LS, Bailey JJ, Childers R, Deal BJ, Hancock EW, et al. Recommendations for the standardization and interpretation of the electrocardiogram: part I: The electrocardiogram and its technology: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society: endorsed by the International Society for Computerized Electrocardiology. Circulation. 2007;115(10):1306-24 PMID: 17322457 DOI: https://doi.org/10.1161/circulationaha.106.180200
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373-498 PMID: 32860505 DOI: https://doi.org/10.1093/eurheartj/ehaa612
Surawicz B, Childers R, Deal BJ, Gettes LS, Bailey JJ, Gorgels A, et al. AHA/ACCF/HRS Recommendations for the Standardization and Interpretation of the Electrocardiogram: Part III: Intraventricular Conduction Disturbances A Scientific Statement From the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol.2009;53(11):976-81 PMID: 19281930 DOI: https://doi.org/10.1016/j.jacc.2008.12.013
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1-39.e14 PMID: 25559473 DOI: https://doi.org/10.1016/j.echo.2014.10.003
Elliott P, Andersson B, Arbustini E, Bilinska Z, Cecchi F, Charron P, et al. Classification of the cardiomyopathies: a position statement from the European Society Of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2008;29(2):270-6 PMID: 17916581 DOI: https://doi.org/10.1093/eurheartj/ehm342
Yaku H, Ozasa N, Morimoto T, Inuzuka Y, Tamaki Y, Yamamoto E, et al. Demographics, management, and in-hospital outcome of hospitalized acute heart failure syndrome patients in contemporary real clinical practice in Japan-observations from the prospective, multicenter Kyoto Congestive Heart Failure (KCHF) registry. Circ J. 2018;82:2811-9 PMID: 30259898 DOI: https://doi.org/10.1253/circj.cj-17-1386
Mitani H, Funakubo M, Sato N, Murayama H, Rached RA, Matsui N, et al. In-hospital resource utilization, worsening heart failure, and factors associated with length of hospital stay in patients with hospitalized heart failure: A Japanese database cohort study. J Cardiol. 2020;76(4):342-9 PMID: 32636125 DOI: https://pubmed.ncbi.nlm.nih.gov/32636125/
Yu Y, Gupta A, Wu C, Masoudi FA, Du X, Zhang J, et al. Characteristics, Management, and Outcomes of Patients Hospitalized for Heart Failure in China: The China PEACE Retrospective Heart Failure Study. J Am Heart Assoc. 2019;8(17):e012884 PMID: 31431117 DOI: https://doi.org/10.1161/jaha.119.012884
Aune D, Schlesinger S, Norat T, Riboli E. Tobacco smoking and the risk of heart failure: A systematic review and meta-analysis of prospective studies. Eur J Prev Cardiol. 2019;26(3):279-88 PMID: 30335502 DOI: https://doi.org/10.1177/2047487318806658
Nieminen MS, Brutsaert D, Dickstein K, Drexler H, Follath F, Harjola VP, et al. Euro Heart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J. 2006;27(22):2725-36 PMID: 17000631 DOI: https://doi.org/10.1093/eurheartj/ehl193
Steinberg BA, Zhao X, Heidenreich PA, Peterson ED, Bhatt DL, Cannon CP, et al. Trends in patients hospitalized with heart failure and preserved left ventricular ejection fraction: prevalence, therapies, and outcomes. Circulation. 2012;126(1):65-75 PMID: 22615345 DOI: https://doi.org/10.1161/circulationaha.111.080770
Al-Tamimi MA-A, Gillani SW, Abd Alhakam ME and Sam KG. Factors Associated With Hospital Readmission of Heart Failure Patients. Front Pharmacol. 2021;12(0):732760 PMID: 34707497 DOI: https://doi.org/10.3389/fphar.2021.732760
Amran IM, Alias SA, Shahril NS, Basuki HF, Salleh AZZ, Khalil FA, et al. Heart Failure Admissions and its Associated Factors, Complications and Treatment. International Journal of Cardiology. 2019;297(Suppl):22-23 DOI: https://doi.org/10.1016/j.ijcard.2019.11.062
Cleland J, Dargie H, Hardman S, McDonag T, Mitchell P. National Heart Failure Audit, April 2012-March 2013. London: National Institute For cardiovascular Outcomes research (NICOR), Institute of Cardiovascular Science, University College; 2013 Nov. 86p. (Accessed on: 25th July 2022) Available from: http://www.wales.nhs.uk/sitesplus/documents/862/National%20Heart%20Failure%20Audit%20April%202012-March2013.pdf
Lawson CA, Zaccardi F, Squire I, Ling S, Davies MJ, Lam CSP, et al. 20-year trends in cause-specific heart failure outcomes by sex, socioeconomic status, and place of diagnosis: a population-based study. Lancet Public Health. 2019;4(8):e406-e420 PMID: 31376859 DOI: https://doi.org/10.1016/s2468-2667(19)30108-2
Downloads
Published
Issue
Section
License
- The Journal of Lumbini Medical College (JLMC) publishes open access articles under the terms of the Creative Commons Attribution (CC BY) License which permits use, distribution and reproduction in any medium, provided the original work is properly cited.
- JLMC requires an exclusive licence to publish the article first in its journal in print and online.
- The corresponding author should read and agree to the following statement before submission of the manuscript for publication,
- License agreement
- In submitting an article to Journal of Lumbini Medical College (JLMC) I certify that:
- I am authorized by my co-authors to enter into these arrangements.
- I warrant, on behalf of myself and my co-authors, that:
- the article is original, has not been formally published in any other peer-reviewed journal, is not under consideration by any other journal and does not infringe any existing copyright or any other third party rights;
- I am/we are the sole author(s) of the article and have full authority to enter into this agreement and in granting rights to JLMC are not in breach of any other obligation;
- the article contains nothing that is unlawful, libellous, or which would, if published, constitute a breach of contract or of confidence or of commitment given to secrecy;
- I/we have taken due care to ensure the integrity of the article. To my/our - and currently accepted scientific - knowledge all statements contained in it purporting to be facts are true and any formula or instruction contained in the article will not, if followed accurately, cause any injury, illness or damage to the user.
- I, and all co-authors, agree that the article, if editorially accepted for publication, shall be licensed under the Creative Commons Attribution License 4.0. If the law requires that the article be published in the public domain, I/we will notify JLMC at the time of submission, and in such cases the article shall be released under the Creative Commons 1.0 Public Domain Dedication waiver. For the avoidance of doubt it is stated that sections 1 and 2 of this license agreement shall apply and prevail regardless of whether the article is published under Creative Commons Attribution License 4.0 or the Creative Commons 1.0 Public Domain Dedication waiver.
- I, and all co-authors, agree that, if the article is editorially accepted for publication in JLMC, data included in the article shall be made available under the Creative Commons 1.0 Public Domain Dedication waiver, unless otherwise stated. For the avoidance of doubt it is stated that sections 1, 2, and 3 of this license agreement shall apply and prevail.
Please visit Creative Commons web page for details of the terms.